Can lupus nephritis disease activity and renal flares be tracked non-invasively with urine biomarkers?
Lead: Ting Zhang
Team members: Kamala Vanarsa
Collaborator: Drs. Petri, Saxena, Pedroza
Project Summary:
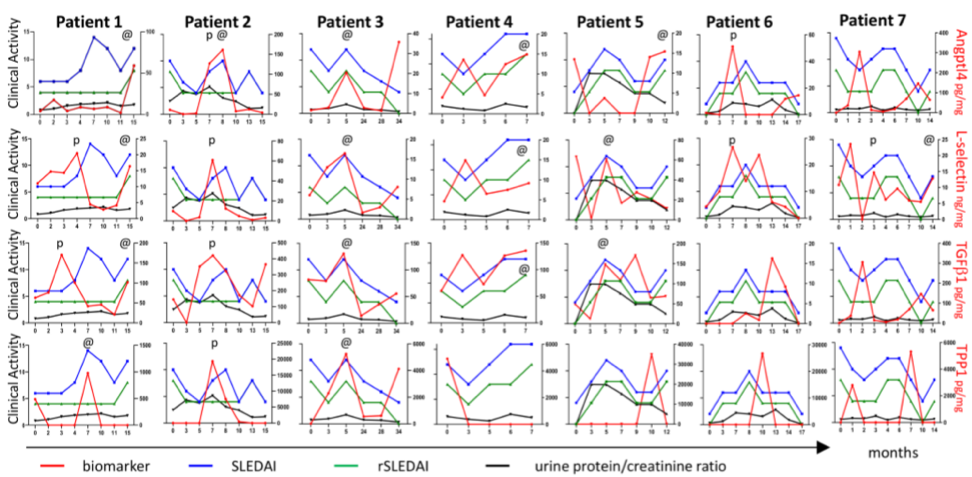
To address whether lupus nephritis (LN) disease activity and renal flares can be tracked non-invasively using urine biomarkers, the performance of the top biomarker candidates identified via an unbiased planar array screen in patients with LN in our previous studies were evaluated in a discovery cohort of LN patients with serial follow-up visits. Urine Angptl4, L-selectin, TGFβ1, and TPP1 were measured in 7 LN patients over multiple hospital visits. The serial tracking plots demonstrate the fluctuations of these proteins along with SLEDAI, rSLEDAI, and urine protein-to-creatinine (UrPrCr) ratio over time. In some visits, these proteins rose simultaneously (marked with “@”) with the increase of disease activity as reflected by the SLEDAI or rSLEDAI indices or UrPrCr ratio, while in other visits, these proteins rose preceding the clinical flare (marked using “p”). Of the 4 urine proteins tested, urine L-selectin preceded or coincided with worsening of SLEDAI or rSLEDAI in all 7 patients. Urine Angptl4 also performed well, preceding or coinciding with worsening of SLEDAI or rSLEDAI in 6 of 7 patients. Urine TGFβ1 ranked third, as it preceded or coincided with worsening of SLEDAI or rSLEDAI in 5 of 7 patients. In all cases, the fluctuations in urine biomarkers were substantially more pronounced than the subtle changes in proteinuria.
What is already known in the field?
- The incidence of renal flares varies from 22% to 66% in LN, and these contribute substantially to morbidity and mortality in SLE. While proteinuria is widely used as a diagnostic parameter in LN, proteinuria cannot differentiate between disease activity and damage. Urinary biomarkers which are able to predict flares of LN are of great utility in management of LN.
What is new?
- Urine L-selectin and TPP-1 were independent predictors of SLEDAI, whereas urine L-selectin, Angptl4 and TGFb1 were independent predictors of rSLEDAI.
- Urine L-selectin was best at predicting an oncoming rise in rSLEDAI (within the following 1-2 months), with Angptl4 and TGFb1 being almost as predictive.
- Urine Angptl4 was best at predicting oncoming increases in SLEDAI (within the following 1-2 months), with L-selectin and TGFb1 being almost as predictive.
Why is this important?
- These biomarker proteins rose simultaneously with or preceded the increase in disease activity, more prominently and sometimes earlier than proteinuria. Hence, these easily measurable urine proteins hold promise in tracking LN patients serially during follow-up. This is important because early detection of renal flares and prompt treatment improves disease outcome in patients with LN. Moreover, unlike the renal biopsy, urine markers can be serially monitored, and can even be performed by the patient from home.
Ongoing/future steps:
- Expand the longitudinal LN patient cohort (with flares during follow-up), and evaluate the performance of these novel biomarkers in predicting disease flares and long-term outcomes.
- To compare the performance of different urine biomarkers to assess which biomarkers perform best, individually or together, in LN patients of different ethnicities.